■ ■ ■ Description
The meniscus is a cartilage structure in the knee that sits on top of the leg bone (tibia). Each knee has two menisci, an inner and an outer meniscus. The meniscus functions like an adaptor between the rounded thigh bone (femur) and flat tibia. It also serves to help distribute the forces between the two bones over a greater area (rather than point to point), helps supply nutrition to the cartilage that lines the bones (articular cartilage), and helps stabilize the knee. A discoid meniscus is a congenital (born with) variant of the normal meniscus. Instead of being shaped like a cashew nut, the meniscus is more oval or disk shaped. Occasionally it has a normal shape with abnormal attachment to the surrounding structures. It tends to occur in the outer (lateral) meniscus. The meniscus may cause symptoms without injury or can cause symptoms when torn or injured.
■ ■ ■ Common Signs and Symptoms
-
Often, no symptoms at all
-
Snapping or clunking of the knee with motion
-
Pain, especially with standing on the affected leg, and tenderness along the joint of the knee
-
Swelling of the affected the knee noted 1 to 2 days after the injury, although it may occur right after the injury
-
Locking of the knee (cannot straighten the knee completely)
-
Giving way or buckling of the knee
■ ■ ■ Causes
The cause is unknown, but discoid meniscus is thought to be a developmental or congenital problem (you are born with it). It can occur in both knees in up to 10% of people with this condition.
■ ■ ■ Risk Increases With
-
Contact sports (football), as well as sports in which cleats are involved with pivoting (soccer), or sports in which good shoe grip and sudden change in direction are required (racquetball, basketball)
-
Previous knee injury
-
Associated knee injury, particularly ligament injuries
-
Poor physical conditioning (strength and flexibility)
-
Caucasians have a low incidence of this problem (up to 5%), whereas it occurs in up to 25% of Asians.
■ ■ ■ Preventive Measures
-
Appropriately warm up and stretch before practice or competition.
-
Maintain appropriate conditioning:
-
Cardiovascular fitness
-
Knee strength
-
Flexibility and endurance
-
-
For participation in jumping (basketball, volleyball) or contact sports, protect the knee joint with supportive devices, such as wrapped elastic bandages, tape, or braces (these have not been proven effective).
-
Wear proper protective equipment and ensure correct fit, including proper cleats for the surface.
■ ■ ■ Expected Outcome
Some meniscal injuries can heal on their own, and some do not heal but may not cause any symptoms. However, the only definitive treatment for meniscal tears requires surgery. Surgery may provide complete healing in 6 weeks. If there are no symptoms, there is no known problem with leaving the meniscus alone (no surgery).
■ ■ ■ Possible Complications
-
Frequent recurrence of symptoms, resulting in a chronic problem; appropriately addressing the problem the first time decreases frequency of recurrence
-
Repeated knee injury, particularly if sports are resumed too soon after injury or surgery
-
Progression of the tear (it gets larger) if untreated
-
Arthritis of the knee in later years (with removal of tear or without surgery)
-
Complications of surgery, including infection, bleeding, injury to nerves (numbness, weakness, paralysis) continued pain, giving way, locking, need for further surgery, and knee stiffness (loss of motion)
■ ■ ■ General Treatment Considerations
If the discoid meniscus is found incidentally and does not cause symptoms, nothing needs to be done. If injured, initial treatment consists of medications and ice to relieve pain and reduce the swelling of the affected joint. Sometimes walking with crutches until you walk without a limp is recommended (you may put full weight on the injured leg). Range-of-motion, stretching, and strengthening exercises may be carried out at home, although referral to a physical therapist or athletic trainer may be recommended. Occasionally your physician may recommend a brace or immobilizer or crutches to protect the joint. Arthroscopic surgery is often recommended as definitive treatment. Usually the tear is removed, although occasionally a repair may be attempted. After surgery or immobilization, stretching and strengthening of the injured, stiff, and weakened joint and surrounding muscles are necessary. These may be done with or without the assistance of a physical therapist.
■ ■ ■ Medication
-
Nonsteroidal anti-inflammatory medications, such as aspirin and ibuprofen (do not take within 7 days before sur- gery), or other minor pain relievers, such as acetaminophen, are often recommended. Take these as directed by your physician. Contact your physician immediately if any bleeding, stomach upset, or signs of an allergic reaction occur.
-
Pain relievers may be prescribed as necessary by your physician. Use only as directed and only as much as you need.
■ ■ ■ Heat and Cold
-
Cold is used to relieve pain and reduce inflammation for acute and chronic cases. Cold should be applied for 10 to 15 minutes every 2 to 3 hours for inflammation and pain and immediately after any activity that aggravates your symptoms. Use ice packs or an ice massage.
-
Heat may be used before performing stretching and strengthening activities prescribed by your physician, physical therapist, or athletic trainer. Use a heat pack or a warm soak.
■ ■ ■ Notify Our Office If
-
Symptoms get worse or do not improve in 2 weeks despite treatment
-
New, unexplained symptoms develop (drugs used in treatment may produce side effects)

➢RANGE OF MOTION AND STRETCHING EXERCISES • Discoid Meniscus
Following surgery, immobilization, or the onset of symptoms, these are some of the initial exercises you may start your rehabilitation program with until you see your physician, physical therapist, or athletic trainer again or until your symptoms are resolved. Please remember:
-
Flexible tissue is more tolerant of the stresses placed on it during activities.
-
Each stretch should be held for 20 to 30 seconds.
-
A gentle stretching sensation should be felt. If any sharp, pinching sensation is felt in the knee, stop
these exercises.
RANGE OF MOTION • Knee Extension, Prone
-
Lie on your stomach on a bed or sturdy table with your knee and leg off the table. The kneecap should be off the edge of the bed or table.
-
Allow gravity to straighten your knee for you.
-
Hold this position for _____ seconds.
-
Repeat exercise _____ times, ______ times per day.
Note: If authorized by your physician, physical therapist, or athletic trainer, you may place a _____ weight on your ankle to obtain a more effective stretch.


RANGE OF MOTION • Gravity Knee Flexion
-
Lie on the floor as shown with your toes/foot lightly touching the wall.
-
Allow your toes/foot to slide down the wall, allowing gravity to bend your knee for you.
-
Obtain a “comfortable” stretching sensation.
-
Hold this position for _____ seconds. Then return the leg to the starting position.
-
Repeat exercise _____ times, ______ times per day.
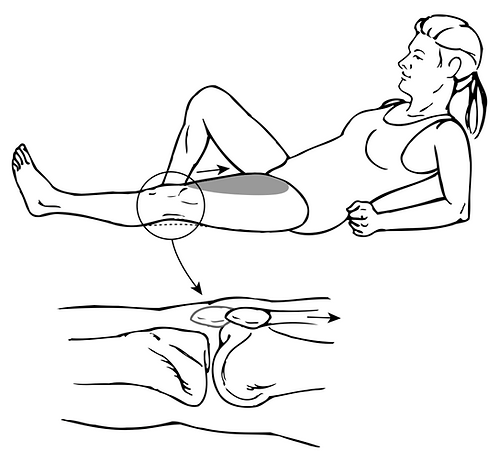
FLEXIBILITY • Hamstrings
-
Lie on your back with your leg bent and both hands holding on to it behind the thigh as shown.
-
Your hip should be bent to 90 degrees and the thigh pointing straight at the ceiling.
-
Straighten out your knee as far as you can. Keep your thigh pointing straight toward the ceiling.
-
Keep the other leg flat on the floor.
-
Hold this position for _____ seconds.
-
Repeat exercise _____ times, ______ times per day.

➢STRENGTHENING EXERCISES • Discoid Meniscus
Following surgery, immobilization, or the onset of symptoms, these are some of the initial exercises you may start your rehabilitation program with until you see your physician, physical therapist, or athletic trainer again or until your symptoms are resolved. Please remember:
-
Strong muscles with good endurance tolerate stress better.
-
Do the exercises as initially prescribed by your physician, physical therapist, or athletic trainer. Progress slowly with each exercise, gradually increasing the number of repetitions and weight used under their guidance.
STRENGTH • Quadriceps, Isometrics
-
Lie flat or sit with your leg straight.
-
Tighten the muscle in the front of your thigh as much as you can, pushing the back of your knee flat against the floor. This will pull your kneecap up your thigh, toward your hip.
-
Hold the muscle tight for _____ seconds.
-
Repeat this exercise _____ times, ______ times per day.

STRENGTH • Quadriceps, Short Arcs
-
Lie flat or sit with your leg straight.
-
Place a _____ inch roll under your knee, allowing it to bend.
-
Tighten the muscle in the front of your knee as much as you can, and lift your heel off the floor.
-
Hold this position for _____ seconds.
-
Repeat exercise _____ times, ______ times per day.
Additional Weights: OK TO USE DO NOT USE!!!
If okay’d by your physician, physical therapist, or athletic trainer, a ____ pound weight may be placed around your ankle for additional weight.

STRENGTH • Quadriceps, 7 Count
The quality of the muscle contraction in this exercise is what counts the most, not just the ability to lift your leg!
-
Tighten the muscle in front of your thigh as much as you can, pushing the back of your knee flat against the floor.
-
Tighten this muscle harder.
-
Lift your leg/heel 4 to 6 inches off the floor.
-
Tighten this muscle harder again.
-
Lower your leg/heel back to the floor. Keep the muscle in front of your thigh as tight as possible.
-
Tighten this muscle harder again.
-
Relax.
-
Repeat exercise _____ times, ______ times per day.
View as PDF