Tibial Eminence Fracture
■ ■ ■ Description
A tibial eminence fracture is a partial or complete fracture of the attachment of the anterior cruciate ligament (ACL), one of the four major ligaments of the knee. The ACL is a ropelike structure that helps keep the normal relationship of the femur (thigh bone) and the tibia (leg bone). This ligament is most important in sports that require pivoting, changing direction (cutting), or jumping and landing. In children the bony attachment of the ACL is more likely to break off (fracture) than the ligament is to tear (sprain). However, this ligament is often stretched in conjunction with the bone pulling off the leg bone (tibia). This is because the bony attachment connects to the leg bone via growth plate cartilage, which is weaker than the ligament. Associated injuries to the collateral ligaments (on either side of the knee) or the meniscus cartilage occur often with this injury.
■ ■ ■ Common Signs and Symptoms
-
Pop or tear heard or felt at the time of injury
-
Large knee swelling noticed almost immediately (within 3 hours)
-
Inability to straighten knee
-
Pain around the knee and difficulty standing on the leg
-
Knee giving way or buckling, particularly when trying to pivot, cut (rapidly change direction), or jump; often, swelling with repeated giving way
-
Occasionally, locking when there is concurrent injury to the meniscus cartilage
■ ■ ■ Causes
A tibial eminence fracture is caused by force that exceeds the strength of the growth plate. This injury may be as a result of a noncontact injury (landing awkwardly or cutting while cleats are stuck to the ground) or from contact, such as getting tackled at the knee.
■ ■ ■ Risk Increases With
-
Sports that require pivoting, jumping, cutting, or changing direction (basketball, soccer, volleyball) or contact sports (football, rugby)
-
Poor physical conditioning (strength and flexibility)
-
Athletes under 14 years of age
-
Improper equipment
■ ■ ■ Preventive Measures
-
Appropriately warm up and stretch before practice and competition.
-
Maintain appropriate conditioning:
-
Thigh, leg, and knee flexibility
-
Muscle strength and endurance
-
Cardiovascular fitness
-
-
Use proper technique.
-
Wear proper equipment (such as the correct length of cleats for the surface).
■ ■ ■ Expected Outcome
The bone will usually heal with appropriate treatment, although residual knee looseness and giving way may occur, especially with sports that require pivoting, cutting, and jumping and landing.
■ ■ ■ Possible Complications
-
Failure to heal (nonunion)
-
Healing in a poor position (malunion)
-
Frequent recurrence of symptoms, such as knee giving way, instability, and swelling
-
Injury to meniscal cartilage, resulting in locking and swelling of the knee
-
Arrest of normal bone growth in children
-
Injury to other structures of the knee, including the articular cartilage, resulting in arthritis of the knee
-
Injury to other ligaments of the knee
-
Knee stiffness (loss of knee motion)
-
Risks of surgery, including infection, bleeding, injury to nerves (numbness, weakness, paralysis), and need for further surgery (ACL reconstruction)
■ ■ ■ General Treatment Considerations
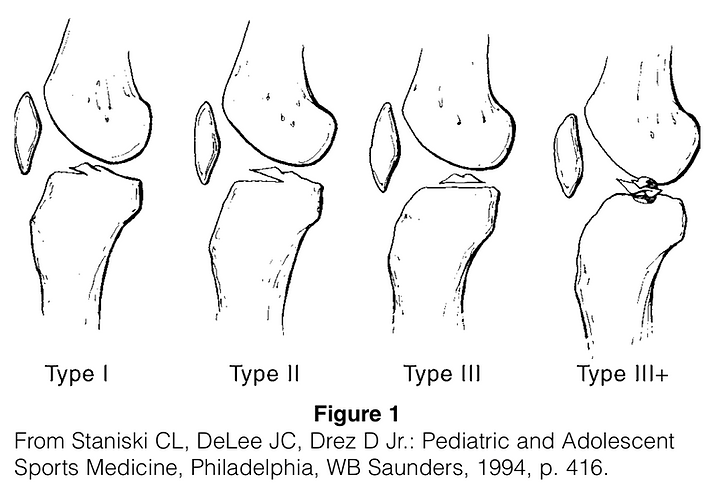
Initial treatment consists of medications and ice to relieve pain and reduce the swelling of the knee. If the bone is in the proper position or can be positioned without surgery, immobilization with a brace or cast for 4 to 6 weeks is recommended. Crutches may be recommended for walking. If the bones are not in proper position, surgery is usually needed to reposition the bones and hold them with sutures, wires, or screws. After immobilization (with or without surgery), stretching and strengthening of the injured and weakened joint and surrounding muscles (due to the injury and the immobilization) are necessary. These may be done with or without the assistance of a physical therapist or athletic trainer. The sutures, wires, or screws usually do not need to be removed.
■ ■ ■ Medication
-
Nonsteroidal anti-inflammatory medications, such as aspirin and ibuprofen (do not take within 7 days before surgery), or other minor pain relievers, such as acetaminophen, are often recommended. Take these as directed by your physician. Contact your physician immediately if any bleeding, stomach upset, or signs of an allergic reaction occur.
-
Stronger pain relievers may be prescribed as necessary by your physician. Use only as directed.
■ ■ ■ Heat and Cold
-
Cold is used to relieve pain and reduce inflammation. Cold should be applied for 10 to 15 minutes every 2 to 3 hours for inflammation and pain and immediately after any activity that aggravates your symptoms. Use ice packs or an ice massage.
-
Heat may be used before performing stretching and strengthening activities prescribed by your physician, physical therapist, or athletic trainer. Use a heat pack or a warm soak.
■ ■ ■ Notify Our Office If
-
Symptoms get worse or do not improve
-
You experience pain, numbness, or coldness in the foot
-
Blue, gray, or dusky color appears in the toenails
-
Any of the following occur after surgery: fever, increased pain, swelling, redness, drainage, or bleeding in the surgical area
-
New, unexplained symptoms develop (drugs used in treatment may produce side effects)
View as PDF